Phlebitis Diagnosis: Understanding and Managing Vascular Health

Phlebitis is a condition characterized by the inflammation of a vein, often occurring in the legs. This condition can lead to severe complications if not diagnosed and treated promptly. In this comprehensive article, we will delve into the various aspects of phlebitis diagnosis, covering its symptoms, causes, risk factors, and treatment options. By understanding this prevalent condition better, both patients and healthcare professionals can ensure effective management and optimal health outcomes.
What is Phlebitis?
Phlebitis refers to the inflammation of a vein, which can manifest as either superficial or deep vein issues. Superficial phlebitis affects veins near the surface of the skin, while deep vein phlebitis (or deep vein thrombophlebitis) occurs in deeper veins, posing a greater risk of complications such as deep vein thrombosis (DVT). Understanding the distinction between these two types is critical for accurate diagnosis and treatment.
Symptoms of Phlebitis
The symptoms of phlebitis can range from mild to severe, depending on the type and location of the affected vein. Common symptoms include:
- Redness and warmth over the affected vein.
- Swelling in the area surrounding the inflamed vein.
- Pain or tenderness along the vein route.
- Hardness or a cord-like feeling under the skin.
- Skin discoloration near the affected area.
It is essential to note that symptoms can vary, and some individuals may experience no symptoms at all. However, if you notice any of these signs, seeking medical advice is crucial.
Causes of Phlebitis
Phlebitis can arise from several factors, including:
- Injury or trauma to a vein, such as from surgery or intravenous (IV) lines.
- Prolonged immobility, which can occur during long flights or bed rest.
- Blood clots that develop in veins, leading to inflammation.
- Infections that affect the veins or tissues around them.
- Certain medical conditions that increase blood clotting, such as cancer or autoimmune disorders.
Risk Factors for Phlebitis
Several factors can increase the risk of developing phlebitis:
- Age: Older adults are at higher risk due to decreased vein elasticity.
- Obesity: Excess weight increases pressure on veins in the legs.
- Smoking: Tobacco use affects blood circulation and can contribute to vein inflammation.
- Family history: A family history of venous diseases may predispose individuals to phlebitis.
- Certain medications: Hormone replacement therapy or contraceptives can elevate the risk.
Phlebitis Diagnosis: Steps to Take
The phlebitis diagnosis process typically involves a comprehensive evaluation by a healthcare professional. Below are the steps usually taken:
1. Medical History Review
The physician will begin by taking a detailed medical history, including:
- Previous health issues, especially related to vein and blood clots.
- Current symptoms, their duration, and severity.
- Medication history, including over-the-counter drugs and supplements.
2. Physical Examination
A thorough physical examination will follow. The healthcare provider will:
- Inspect the affected area for signs of inflammation.
- Palpate the vein to check for tenderness or hardness.
- Assess for swelling or any signs of complications, such as skin changes.
3. Diagnostic Imaging
Depending on the examining physician’s findings, further diagnostic imaging may be necessary, including:
- Ultrasound: This is the most common and effective method for diagnosing phlebitis, allowing visualization of blood flow and vein condition.
- Venography: In rare cases, a contrast dye may be injected into the veins to enhance imaging results.
Treatment Options for Phlebitis
Once diagnosed, the treatment for phlebitis will depend on its severity and the patient’s overall health. Common treatment methods include:
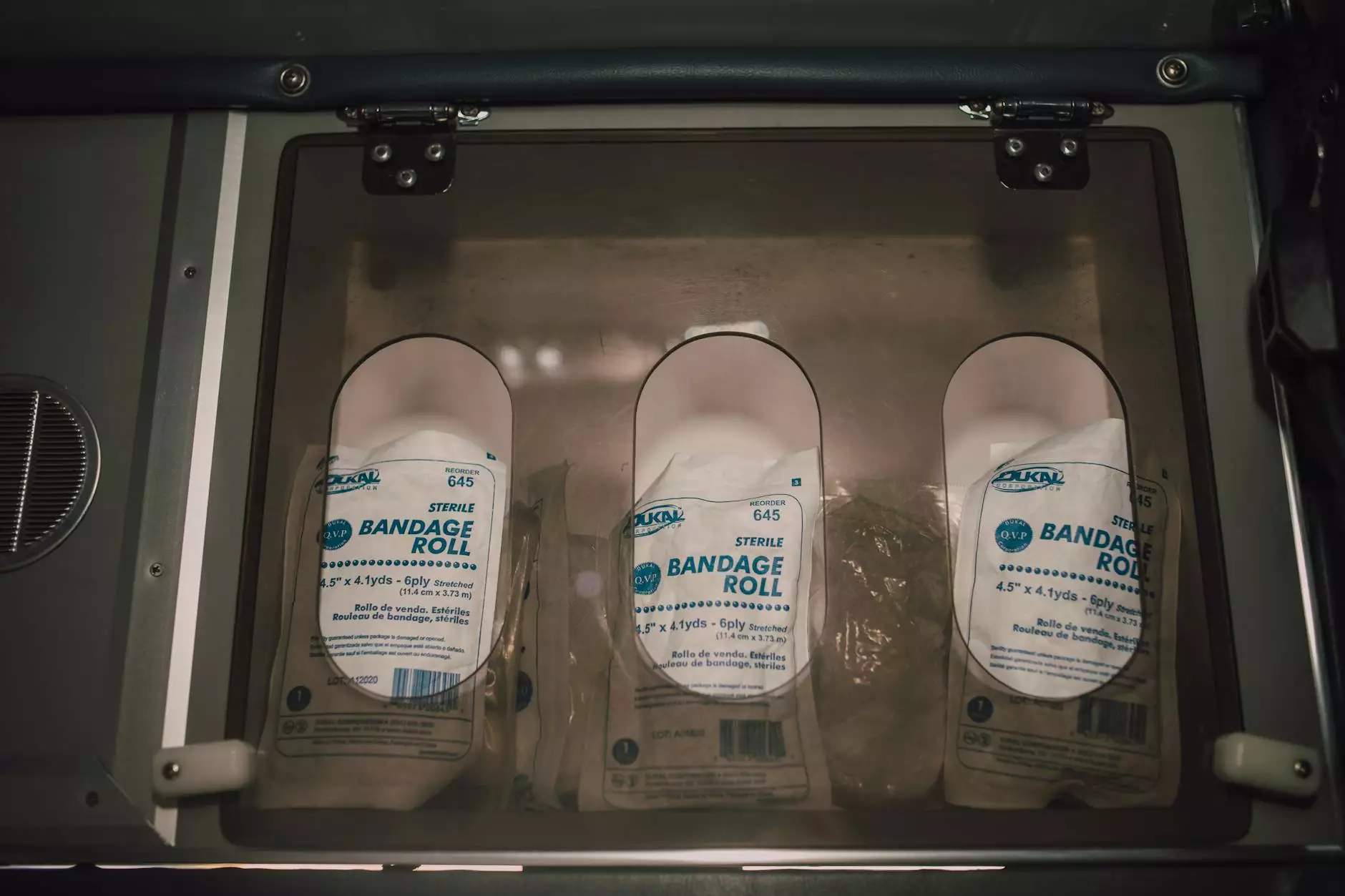
1. Medications
Medications play a crucial role in managing phlebitis. Commonly prescribed medications include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These help reduce pain and inflammation.
- Anticoagulants: If a blood clot is present, these medications help thin the blood and prevent further clotting.
2. Compression Therapy
Compression stockings are often recommended to help manage symptoms of phlebitis. They work by:
- Improving blood flow in the legs.
- Reducing swelling and discomfort.
3. Lifestyle Changes
Making certain lifestyle changes can significantly improve vascular health and reduce the risk of phlebitis:
- Regular exercise: Engaging in physical activity enhances circulation.
- Healthy diet: A diet rich in fruits, vegetables, and whole grains contributes to vascular health.
- Avoiding prolonged immobility: Take frequent breaks to move and stretch, especially during long periods of sitting.
4. Surgical Intervention
In severe cases, particularly where there is a risk of serious complications or persistent symptoms, surgical intervention may be necessary. Options can include:
- Vein stripping or ligation: Removal of the affected vein to alleviate symptoms.
- Endovenous laser treatment (EVLT): A minimally invasive procedure that uses laser energy to close off affected veins.
Prevention of Phlebitis
Rather than focusing solely on treatment, prevention of phlebitis is crucial. Here are some effective strategies:
- Stay active: Regular exercise promotes healthy circulation.
- Maintain a healthy weight: Reducing obesity lowers the strain on veins.
- Hydration: Keeping hydrated is important for overall vascular health.
- Consult healthcare providers: If at risk, discuss with your doctor appropriate preventive strategies, especially if you plan to undergo surgical procedures or travel long distances.
Conclusion
Understanding and managing phlebitis diagnosis is essential for maintaining vascular health. Early detection and treatment can prevent complications such as deep vein thrombosis and pulmonary embolism. By recognizing the symptoms, risk factors, and available treatments, patients can take proactive steps towards better health.
At Truffles Vein Specialists, our team of experienced healthcare professionals is dedicated to providing comprehensive vascular care. If you are experiencing symptoms of phlebitis or have concerns about your vascular health, we encourage you to contact us for a consultation. Your health is our priority, and we are here to support you every step of the way.